The top medical coding and billing courses in Vermont are looking to fill their classrooms and satisfy the growing demand for billers and coders! The allied health field as a whole in Vermont is growing fast every year and the medical insurance coding and billing field is no different. See the details from bls.gov below and much more with our latest free resource.
With the healthcare field field growing due to baby boomers demand for healthcare and our country’s ever growing population we can expect the need for qualified workers to be real strong over time. The medical insurance coder in Vermont will be front and center on that demand due to the fact that they process all the insurance payment information and procedures for all healthcare. They are one of the cogs right in the center of the whole healthcare industry wheel in Vermont.
Becoming a medical coding and billing specialist in Vermont
Medical billers and coders aren’t regulated by the state of Vermont. The industry is regulated at a national level by the associations that listed in detail at the link here. See more details about the certifying bodies and what they do for the industry as a whole not just in Vermont at the link above.
Find Medical Billing and Coding Schools in Vermont
What is the process for becoming a certified biller or coder in Vermont?
For those looking for the steps for becoming a medical biller or coder in Vermont is detailed and summarized in the following four steps listed below.
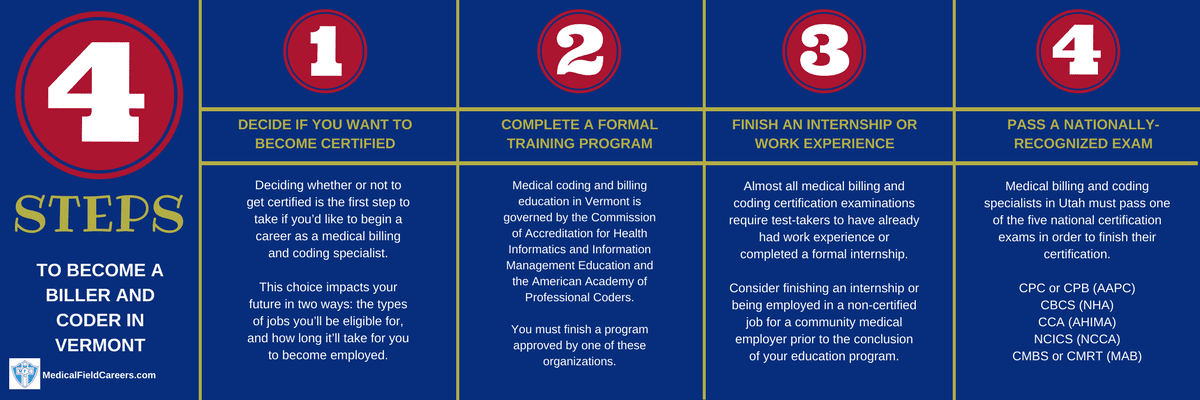
Step 1 – Make the choice if you plan to get a Vermont Billing and Coding certification
Before doing anything else, you’re going to first need to decide if you are going to get a medical billing and coding certification in Vermont, or seek out a job without one. This choice can affect your future in two ways: the kinds of positions you will be allowed to interview for, and how long it’ll take you to become employed in the state of Vermont. Getting your coding certification in Vermont will actually get your career off on the right foot! It cannot be undervalued and will absolutely help you and your career in the short term and long term. Do not let the value of coding certification be undersold or undervalued at any level!
Step 2 – Complete a formal Medical Coding and Billing training program in VT
Medical billing and coding programs give three different types of credentials to graduates. They are an associate-level degree, a bachelor’s degree, and a certificate. Any of these awards could help you secure a medical billing and coding position, but you need to be aware of the benefits and drawbacks of each before choosing one. The time tables for each level of education are as follow: 6 months to 1 year for certificate, 2 years for associates degree and 4 years for bachelors degree. The longer you attend your educational program you will be better off. Each level of education sets you up for differing levels of job quality and certification level.
How to compare coding and billing programs in Vermont
To find the right choice on billing schools for you in Vermont it can be really simple. All you need to do is know what is most important to you. If cost is most important, sort school options by cost and make your decision. It really can be that easy. Do not rush in to your decision, it is really important that you make the best decision possible. Students loans and debt is a huge issue in our country and you do not want to rush in to any decision when it comes to your education costs.
Approved Medical Coding and Billing Training Programs in Vermont
Community College of Vermont – Medical Insurance Coding and Billing Program PO Box 489, Montpelier, VT 05601 800-228-6686
Step 3 – Complete an internship or get work experience
Area companies sometimes work hand in hand with accredited billing and coding programs to help coordinate internships or work experience for students. Nevertheless, it’s a good strategy to figure out whenever possible if your school will help you with this certification test requirement. Internships can not be understated for its value to you and your future in the field of medical coding is great! Internships can change your career trajectory in major ways and make sure you look for those opportunities.
Step 4 – Successfully pass your Vermont coding and billing certification examination
Medical billing and coding specialists in Vermont must pass one of several national certification examinations to receive their certification. The examinations are made up of segments on every main area of knowledge you would’ve studied in your study course. Several of the major national certification assessments administered in Vermont are detailed at the link here. The detailed resource covers the exam preparation that is necessary, what to expect the day of the exam and much more! We wanted to make sure we covered it all in our breakdown of the exam for medical coding and billing certification in Vermont.
Medical coder and biller salary and jobs in Vermont
There’s a higher than average demand for medical billing and coding specialists in Vermont. Through the year 2024, the Bureau of Labor Statistics projects a 8% growth in additional jobs for medical insurance billing and coding specialists in Vermont. Below is a record of the largest metropolitan areas in Vermont and more information on medical coding and billing salary by area and county. All the data that is used in the report below comes from the bls.gov website.
| Location | Pay Type | Low | Median | High |
|---|---|---|---|---|
| United States | Hourly | $12.05 | $18.29 | $30.21 |
| Yearly | $25,070 | $38,040 | $62,840 | |
| Vermont | Hourly | $13.31 | $18.40 | $29.09 |
| Yearly | $27,690 | $38,280 | $60,510 | |
| Burlington-South Burlington, VT Metropolitan NECTA | Hourly | $13.57 | $18.77 | $29.55 |
| Yearly | $28,220 | $39,040 | $61,450 | |
| Southern Vermont BOS | Hourly | $13.11 | $18.40 | $28.75 |
| Yearly | $27,270 | $38,280 | $59,790 | |
| Northern Vermont BOS | Hourly | $13.05 | $17.41 | $24.50 |
| Yearly | $27,140 | $36,200 | $50,960 |

