How to become a medical biller or coder in Utah
Find Medical Billing and Coding Programs in Utah
What is the process for becoming a certified biller or coder in Utah?
The relatively short process for becoming a medical biller or coder in Utah is shown below in the following steps.
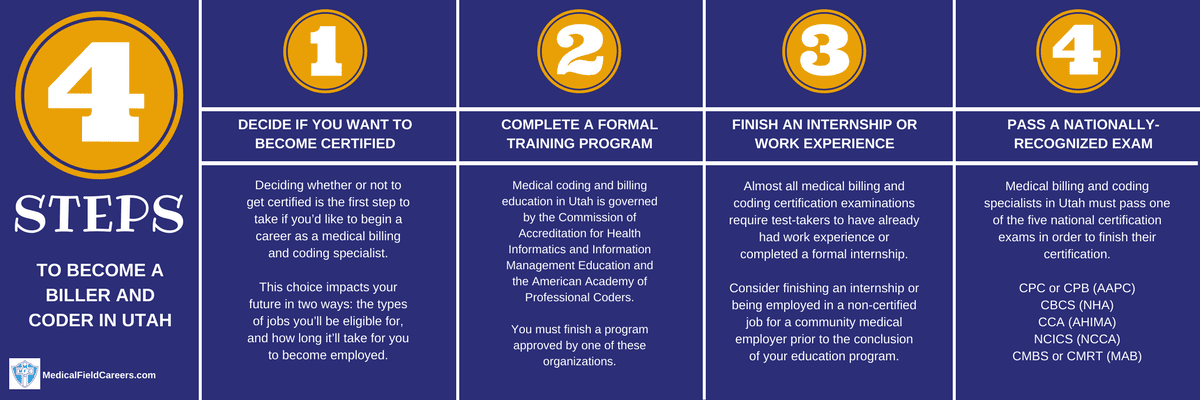
Step 1 – Choose if you are Going to get a Medical Coding Certification in the State of Utah
Step 2 – Finish the Necessary Billing and Coding Training in Utah
Comparing coding and billing programs in Utah
If you are looking at finding a way to select the right program for you in Utah for medical coding or billing, just follow this one rule. Figure out what matters to you most in terms of choosing a school. It can be location, cost or any other factor and if you just stay committed to that factor the right school will find its way to the top of your list.
Approved Coding and Billing Programs in Utah
Below is the full list of Utah medical coding and billing classes.
Weber State University Medical Coding Courses 3850 Dixon Parkway Dr. Dept. 1031 Ogden UT 84408-1031 801-626-6000
Salt Lake Community College Medical Coding Courses 4600 S Redwood Rd Salt Lake City UT 84123 801-957-4111
Ogden-Weber Technical College Medical Coding Courses 200 N Washington Blvd Ogden UT 84404-4089 801-627-8300
Dixie Technical College Medical Coding Courses 1506 S. Silicon Way Saint George UT 84770 435-674-8400
Bridgerland Technical College Medical Coding Courses 1301 North 600 West Logan UT 84321 435-753-6780
Southwest Technical College Medical Coding Courses 757 West 800 South Cedar City UT 84720 435-586-2899
Mountainland Technical College Medical Coding Courses 2301 West Ashton Blvd. Lehi UT 84043 801-753-4100-4100
LDS Business College Medical Coding Courses 95 North 300 West Salt Lake City UT 84101-3500 801-524-8100
Tooele Technical College Medical Coding Courses 88 South Tooele Blvd. Tooele UT 84074-2093 435-248-1800
AmeriTech College-Draper Medical Coding Courses 12257 South Business Park Drive-Ste 100 Draper UT 84020-6545 801-816-1444
Provo College Medical Coding Courses 1450 W 820 N Provo UT 84601 801-818-8901
Step 3 – Accumulate work experience or get Internship in Utah
Step 4 – Finish the Utah coding and billing certification process
Several of the main national certification tests recognized in Utah are shown here. We cover what is on the exam itself, how to prepare for the exam and much much more!
Medical coding and salary salary and jobs in Utah
| Location | Pay Type | Low | Median | High |
|---|---|---|---|---|
| United States | Hourly | $12.05 | $18.29 | $30.21 |
| Yearly | $25,070 | $38,040 | $62,840 | |
| Utah | Hourly | $12.12 | $17.65 | $29.13 |
| Yearly | $25,220 | $36,720 | $60,600 | |
| Salt Lake City, UT MSA | Hourly | $12.24 | $18.55 | $30.07 |
| Yearly | $25,460 | $38,590 | $62,540 | |
| Provo-Orem, UT MSA | Hourly | $12.11 | $17.57 | $28.31 |
| Yearly | $25,180 | $36,550 | $58,880 | |
| Eastern Utah BOS | Hourly | $12.56 | $16.90 | $22.97 |
| Yearly | $26,120 | $35,150 | $47,790 | |
| Logan, UT-ID MSA | Hourly | $12.08 | $15.83 | $28.91 |
| Yearly | $25,130 | $32,920 | $60,130 | |
| Ogden-Clearfield, UT MSA | Hourly | $11.18 | $15.76 | $26.29 |
| Yearly | $23,250 | $32,780 | $54,680 | |
| St. George, UT MSA | Hourly | $12.74 | $15.11 | $18.82 |
| Yearly | $26,510 | $31,430 | $39,150 |

