The accredited options for medical billing and coding courses in South Dakota are detailed below and we cover the ins and outs of training. A medical biller and coder is a key healthcare professional who performs a variety of record-keeping and insurance functions. Allied health professions in South Dakota are seeing tremendous growth and the excitement is great for medical insurance billers and coders too in the state of South Dakota. Below we get in to the details of the growth, how choose the right accredited medical insurance coding and billing program and much more!
Becoming a medical coding and billing specialist in South Dakota
Being certified is not mandatory for employment as a biller or coder in South Dakota. That being said, it is highly recommended to get certified since employers are looking for certified candidates. The national certifying bodies for medical billing and coding specialists in South Dakota and across the country are detailed at the link here.
Find Medical Billing and Coding Schools in South Dakota
What is the process for becoming a certified biller or coder in South Dakota?
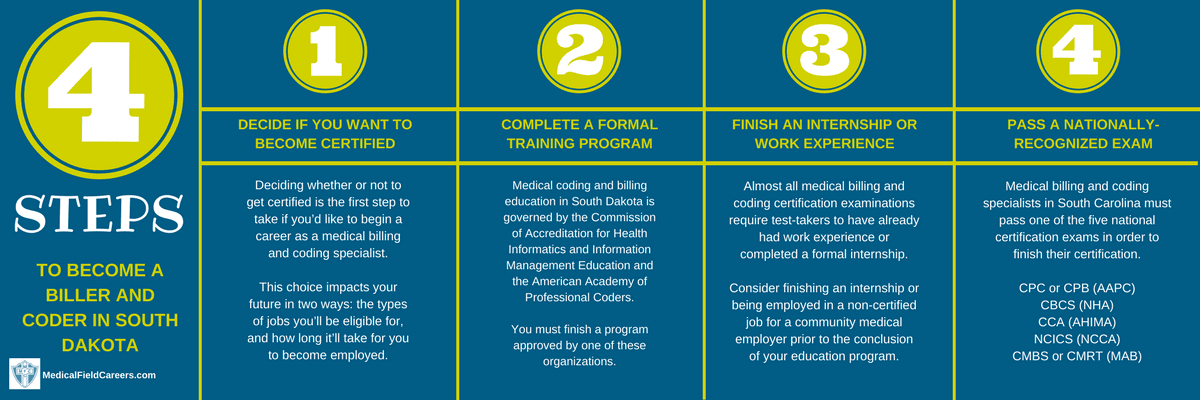
The simple step by step process for becoming a medical biller or coder in South Dakota is detailed in the following steps.
Step 1 – Do you want to get certified as a Medical Coder in South Dakota?
Before anything else, you’ll first have to figure out if you’re going to get a certification in South Dakota, or look for a position without one. This choice could impact your career in a few important ways. One is the type of positions you’ll be eligible to apply for and the other is how long it’s going to take for you to become employed in the state of South Dakota. The path to certification is laid in front of you below and what it can do for you is fantastic! Certification in the state of South Dakota will set your career on the fast track to success! The medical insurance coding and billing certification cannot be undervalued and will tremendously help your career and future in the field!
Step 2 – Complete Medical Billing and Coding Training Program in South Dakota
Medical coding and billing programs award a few types of credentials to graduates: an associate-level degree, a bachelor’s degree, and a diploma (alternately referred to as a “certificate”). Although each credential may qualify you for entry-level medical coding and billing positions, there are several significant differences between the three types of levels of education. The major one is the time tables for each level of education. For instance, it will take 6 months to a full year to get a certificate/diploma in medical coding. It will then take up to 2 years to get an associates degree and around four years if you get your bachelors degree.
How to choose a billing and coding program in South Dakota
To make sure you pick the best school for you, all you have to do is choose based on the factors that are most important to you. It can be that easy if you let it be. If cost is what matters most, than pick the cheapest school in South Dakota that is accredited. If you follow these easy steps, you can avoid choosing the wrong school and you can make your process for choosing a school more streamlined and easier.
Approved Medical Coding and Billing Classes in South Dakota
Below is the list of all the approved medical insurance billing and coding programs in the state of South Dakota.
National American University-Sioux Falls 5801 South Corporate Place Sioux Falls SD 57108-4293 605-336-4600
National American University-Watertown 925 29th Street S.E. Watertown SD 57201-9123 605-884-7200
Southeast Technical Institute 2320 N Career Ave Sioux Falls SD 57107-1301 605-367-7624
Presentation College 1500 N Main Aberdeen SD 57401-1280 605-225-1634
Dakota State University 820 N Washington Ave Madison SD 57042-1799 605-256-5111
National American University-Rapid City 5301 South Highway 16 Rapid City SD 57701-2823 605-394-4800
Step 3 – Get Billing and Coding work experience or Internship in the State of South Dakota
A requirement for many of the South Dakota medical coding and billing certification tests is to have previously acquired job experience or to have completed a formal internship in the state.
Step 4 – Finish the South Dakota Medical Coding and Billing Certification Process
In the State of South Dakota, you are legally required to pass one of the nationally-administered tests for medical billing and coding certification. These assessments incorporate sections on every main area of knowledge you would’ve covered in your formal training course.
The most-popular major national certification examinations administered in South Dakota are detailed at the link here.
Medical coder and biller salary and jobs in South Dakota
In the wonderful state of South Dakota the need is extremely high for medical billing and coding specialists. The Bureau of Labor Statistics (bls.gov) forecasts a fantastic 9% increase in the State of South Dakota through 2024. The list featured below shows information on medical billing and coding specialist compensation in South Dakota by region. All the latest data from the website of bls.gov is used.
| Location | Pay Type | Low | Median | High |
|---|---|---|---|---|
| United States | Hourly | $12.05 | $18.29 | $30.21 |
| Yearly | $25,070 | $38,040 | $62,840 | |
| South Dakota | Hourly | $12.46 | $17.26 | $28.52 |
| Yearly | $25,910 | $35,900 | $59,330 | |
| Western South Dakota BOS | Hourly | $13.60 | $18.12 | $24.15 |
| Yearly | $28,290 | $37,700 | $50,230 | |
| Sioux Falls, SD MSA | Hourly | $12.55 | $17.95 | $32.07 |
| Yearly | $26,100 | $37,340 | $66,700 | |
| Rapid City, SD MSA | Hourly | $12.60 | $17.62 | $27.70 |
| Yearly | $26,200 | $36,650 | $57,620 | |
| Eastern South Dakota BOS | Hourly | $11.83 | $15.53 | $23.67 |
| Yearly | $24,610 | $32,310 | $49,230 | |
| Sioux City, IA-NE-SD MSA | Hourly | $10.92 | $15.15 | $22.12 |
| Yearly | $22,720 | $31,520 | $46,000 |

