If you decide to become a medical billing and coding specialist with accredited medical billing and coding schools in Rhode Island, you will have the opportunity to launch a career in healthcare that is one of the most-popular in the region. The need for qualified allied health workers in Rhode Island is growing and the next decade is shining bright for the healthcare field as a whole and the field of medical insurance coding and billing is absolutely growing fast too. The growth rate gives so much excitement to all aspiring candidates for medical billing and coding training in Rhode Island! Below we cover it in more detail.
Becoming a medical billing and coding specialist in RI
Medical billing and coding specialists in Rhode Island and nationwide are regulated at a national level. The regulating organizations are detailed in depth here. From what to expect to have to do to be eligible to what is on the exams they give, the details are broken down for you at the link above.
Find Medical Billing and Coding Classes in Rhode Island
What is the process for becoming a certified biller or coder in Rhode Island?
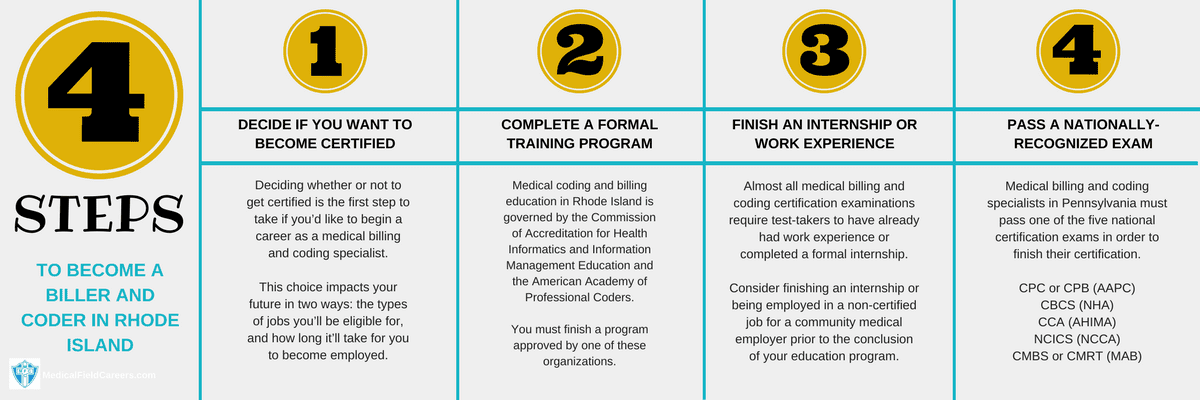
To see the current process for becoming a medical biller or coder in RI is detailed in the following four steps.
Step 1 – Do you want to get certified as a Medical Biller and Coder in Rhode Island?
Prior to doing anything else, you’re going to first want to figure out if you are going to get a medical billing and coding certification, or search for a position without one. There is data to support certification but it is not mandatory that it is earned in Rhode Island. The benefits for medical insurance coding and billing are real strong and cannot be something that is understated. From better pay to better chances at getting hired you will be better served by getting your certification in Rhode Island for medical insurance coding.
Step 2 – Complete a Rhode Island Medical Billing and Coding Training Program
You’ll find a few different types of credentials that may be earned by finishing a formal medical coding and billing training program in the state of Rhode Island. They are certificate/diploma programs, two-year associate degree programs, and a bachelor’s degree program. You can expect a six month to a one year time-frame for certificate/diploma programs, a time-frame of two years for associate degrees and four years for a bachelors degree.
How to decide on a coding and billing program in RI
Picking the right billing and coding classes in Rhode Island is easy as you decide to make it. Some will just go to the closest accredited school and some may make the decision based on multiple factors, or just one factor. Either way, pick the school that works for you based on the factors that matter the most to you individually. Our goal is to make sure you attend the best school for you and we really want the school decision making process to be as easy as we can help make it.
Complete List of Approved Medical Coding and Billing Courses in Rhode Island
Community College of Rhode Island – Medical Coding Courses 400 East Ave Warwick RI 02886-1807 401-825-1000
Step 3 – Acquire Coding and Billing Job Experience or an Internship in Rhode Island
Most of the accredited medical billing and coding schools in Rhode Island make it possible for their pupils to arrange internships with community companies and other companies across the small state of Rhode island. It’s recommended that you speak with your instructor to determine which opportunities are available to let you gain the experience required to be approved for certification assessment. Candidates should look for internships and if they are available, jump on them! They can single handily help your career get off to a great start!
Step 4 – Finish the Coding and Billing certification process in Rhode Island
Medical billing and coding specialists in Rhode Island need to pass one of the five national certification examinations in order to earn their certification. These examinations contain segments on each major area of knowledge you would have studied in your study course.
Several of the major national certification assessments recognized in Rhode Island are put in to deeper detail here. We get in to what to do to prepare for the examination, what to do the day of the examination, what to expect the day of the test and more!
Medical coding and salary salary and jobs in Rhode Island
In Rhode Island, the demand is very high and growing for medical coding and billing specialists! Up through the year 2024, the United States Bureau of Labor Statistics (bls.gov) projects a 6% increase in new positions for medical billing and coding specialists in the great state of Rhode Island. Below is a record of the major metropolitan areas in the state of Rhode Island and more data on medical coding and billing salary by location and county. All the data that is being listed in the table below comes from the latest statistics on the website of the United States Bureau of Labor Statistics.
| Location | Pay Type | Low | Median | High |
|---|---|---|---|---|
| United States | Hourly | $12.05 | $18.29 | $30.21 |
| Yearly | $25,070 | $38,040 | $62,840 | |
| Rhode Island | Hourly | $12.73 | $18.55 | $28.95 |
| Yearly | $26,480 | $38,590 | $60,220 | |
| Norwich-New London, CT-RI Metropolitan NECTA | Hourly | $14.61 | $22.86 | $37.02 |
| Yearly | $30,390 | $47,550 | $77,000 | |
| Providence-Fall River-Warwick, RI-MA Metropolitan NECTA | Hourly | $12.71 | $18.49 | $28.60 |
| Yearly | $26,430 | $38,450 | $59,500 |

