How to become a medical biller or coder in New Jersey
Find Medical Billing and Coding Courses in New Jersey
What is the process for becoming a certified billing and coding specialist in New Jersey?
The simple process for becoming a medical biller or coder in New Jersey is detailed and summarized below in the following four steps.
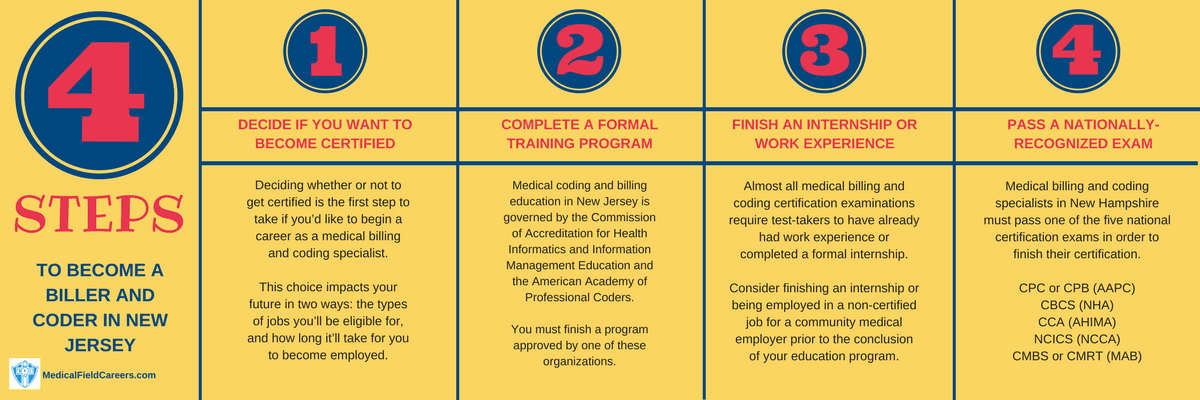
Step 1 – Do you want to get certified as a medical coder in New Jersey?
Step 2 – Finish Your New Jersey Medical Billing and Coding Training
How to choose a billing and coding program in the state of New Jersey
Choose your program of choice and feel confident about it by using the factors that matter to you to choose from the schools in New Jersey.
New Jersey’s Approved Medical Insurance Billing and Coding Programs
American Institute of Medical Sciences & Education Medical Coding Programs 4500 New Brunswick Ave Piscataway NJ 08854 908-222-0002
Rutgers University-New Brunswick Medical Coding Programs 83 Somerset St New Brunswick NJ 08901-1281 732-932-1766
Harris School of Business-Voorhees Campus Medical Coding Programs 401 White Horse Rd. Voorhees NJ 08043 856-309-3701
ASI Career Institute Medical Coding Programs 5360 Black Horse Pike Turnersville NJ 08012-1043 856-232-4677
Lincoln Technical Institute-Paramus Medical Coding Programs 240 Bergen Town Center Paramus NJ 07652-5002 201-845-6868-44500
Branford Hall Career Institute-Jersey City Medical Coding Programs 40 Journal Square, 1st Floor Jersey City NJ 07306 203-672-2300
Passaic County Community College Medical Coding Programs One College Blvd Paterson NJ 07505-1179 973-684-6800
Eastwick College-Nutley Medical Coding Programs 103 Park Ave Nutley NJ 07110 973-661-0600
Salem Community College Medical Coding Programs 460 Hollywood Avenue Carneys Point NJ 08069-2799 856-299-2100
Branford Hall Career Institute-Parsippany Medical Coding Programs 959 Route 46 East Parsippany NJ 07054-3897 203-672-2300
Berkeley College-Woodland Park Medical Coding Programs 44 Rifle Camp Rd Woodland Park NJ 07424 973-278-5400
Harris School of Business-Cherry Hill Campus Medical Coding Programs One Cherry Hill, One Mall Drive Ste.700 Cherry Hill NJ 08002 856-662-5300
Eastwick College-Hackensack Medical Coding Programs 250 Moore Street Hackensack NJ 07601 201-488-9400-5022
Medical Career Institute Medical Coding Programs 901 West Park Avenue Ocean NJ 07712 732-695-1190
American Institute of Medical Sciences & Education Medical Coding Programs 4500 New Brunswick Ave Piscataway NJ 08854 908-222-0002
Fortis Institute-Wayne Medical Coding Programs 201 Willowbrook Blvd. Wayne NJ 07470 973-837-1818-204
Healthcare Training Institute Medical Coding Programs 1969 Morris Ave Union NJ 07083 908-851-7711-110
Fortis Institute-Lawrenceville Medical Coding Programs 2572 Brunswick Pike, Suite 100 Lawrenceville NJ 08648 609-512-2560
Harris School of Business-Hamilton Campus Medical Coding Programs 3620 Quakerbridge Rd Hamilton NJ 08619 609-586-9104
Harris School of Business-Linwood Campus Medical Coding Programs 1201 New Road, Ste 226 Linwood NJ 08221 609-927-4310
Step 3 – Complete an internship or acquire work experience in NJ
Step 4 – Successfully pass coding and billing certification exam in NJ
The most-popular major national certification tests recognized in New Jersey are detailed here. See what to do to efficiently prepare for the certification examination, what to expect the day of the exam itself and more!
Medical billing and coding salary and jobs in New Jersey
| Location | Pay Type | Low | Median | High |
|---|---|---|---|---|
| United States | Hourly | $12.05 | $18.29 | $30.21 |
| Yearly | $25,070 | $38,040 | $62,840 | |
| New Jersey | Hourly | $17.61 | $27.92 | $39.52 |
| Yearly | $36,620 | $58,070 | $82,200 | |
| Newark-Union, NJ-PA Metropolitan Division | Hourly | $18.06 | $28.51 | $41.21 |
| Yearly | $37,560 | $59,310 | $85,720 | |
| Trenton-Ewing, NJ MSA | Hourly | $13.77 | $25.56 | $37.54 |
| Yearly | $28,640 | $53,160 | $78,090 | |
| Camden, NJ Metropolitan Division | Hourly | $16.88 | $23.81 | $34.47 |
| Yearly | $35,110 | $49,520 | $71,710 | |
| Wilmington, DE-MD-NJ Metropolitan Division | Hourly | $13.55 | $18.51 | $28.73 |
| Yearly | $28,170 | $38,510 | $59,750 | |
| Allentown-Bethlehem-Easton, PA-NJ MSA | Hourly | $12.71 | $16.69 | $26.48 |
| Yearly | $26,440 | $34,720 | $55,070 |

