With the allied health industry expanding at an unprecedented pace all around the country, there is plenty of opportunity for people who would like to become a Nevada medical coding and billing specialist with accredited medical coding and billing courses in Nevada. Healthcare careers all across Nevada are growing in demand in big numbers and we will show how medical insurance coders are seeing similar growth. The time could not be more perfect to get in to medical coding and billing field. Bls.gov predicts amazing growth over the next decade and we detail it all for you in our latest free article below.
Becoming a medical billing and coding specialist in Nevada
Billing and coding specialists in Nevada are regulated at a national level by the certifying bodies listed in detail in our article here. It is not mandated to be certified but it is detrimental in many cases not to be.
Find Medical Billing and Coding Programs in Nevada
What is the process for becoming a certified biller or coder in Nevada?
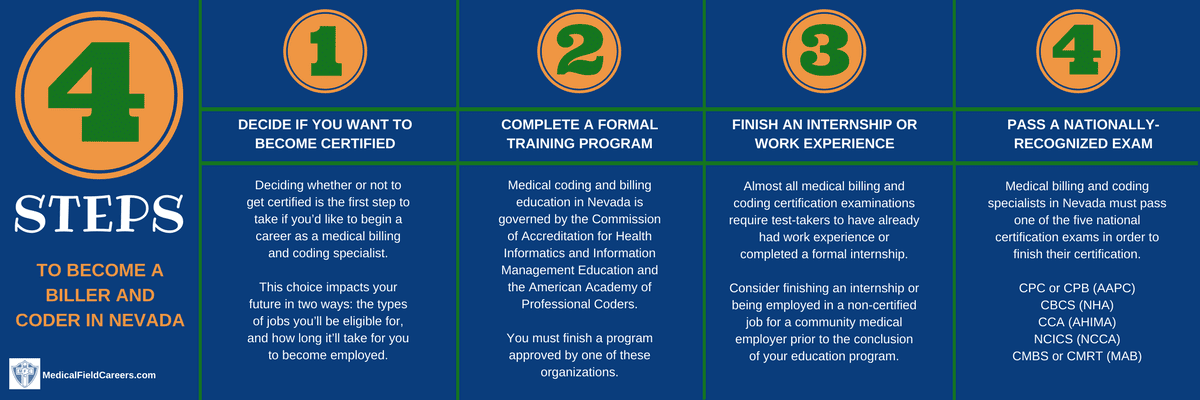
If you are looking at the short process for becoming a medical biller or coder in Nevada, it is summarized in the following four steps.
Step 1 – Do you plan to get certified as a Medical Coder in Nevada?
Before anything else, you will first need to figure out if you are going to get a Nevada medical coding and billing certification. If you do not you will need to start looking for employers that hire non certified medical coders across the state of Nevada. The types of opportunities you’ll be allowed to apply for, and how long it will take for you to get a job are all at a consequence for your choice. The great benefits of getting certified are shown in detailed and they far out shine the downsides of non getting certified. Your career and future will be enhanced by certification greatly.
Step 2 – Complete a formal medical billing and coding training program in NV
The 3 main options for medical coding education in Nevada are all good options and have their own advantages.The options are to earn an associate degree in medical billing and coding, four-year bachelor’s degree, or a certificate. If you take a certificate program, expect 6-12 months of education. If you get an associates degree, expect 2 years education and expect 4 years for a bachelors degree.
Comparing billing and coding programs in Nevada
To figure out which program is best for you with a system that is simple and easy. Think about which factors matter the most to you personally. Whether it is the cost of education, the location or any other matter, just be clear on the factors. Then, sort all the schools in Nevada by those factors and the best option for you will present it itself to you.
Approved Medical Billing and Coding Schools in Nevada
College of Southern Nevada 6375 W. Charleston Blvd. Las Vegas NV 89146-1164 702-651-5000
Great Basin College 1500 College Parkway Elko NV 89801 775-738-8493
Nevada Career Institute 3231 North Decatur Boulevard Las Vegas NV 89130 702-893-3300
Carrington College-Las Vegas 5740 S. Eastern Ave., Ste. 140 Las Vegas NV 89119 702-688-4300
Carrington College-Reno 5580 Kietzke Ln. Reno NV 89511 775-335-2900
Northwest Career College 7398 Smoke Ranch Road, Ste 100 Las Vegas NV 89128 702-254-7577
Step 3 – Complete an internship in Nevada or acquire work experience in billing and coding
Some of the coding and billing certification exams offered in Nevada require you to have completed an internship or complete a specified amount of work experience in advance of becoming approved to sit for testing. Be sure to check with each respective coding and billing program in Nevada if they offer such programs to their students. An internship cannot be undervalued in anyway due to its power in getting you prepared for the career and the tasks expected of you on the job as a medical coder and biller.
Step 4 – Complete the official Nevada billing and coding certification process
In Nevada, you will be legally required to pass one of the nationally-recognized exams for medical billing and coding certification. The tests incorporate segments on all principal areas of knowledge you would’ve studied in your course. Some of the major national certification tests administered in Nevada are detailed at length at this link here. We get in to in-depth detail about exam preparation, what to expect on the examination, what to do the day of the test and much more!
Medical billing and coding salary and jobs in Nevada
The need for medical coding and billing specialists is at record levels in the great state of Nevada. The Bureau of Labor Statistics forecasts a 15% increase in brand new jobs across the country and a 27% increase in the State of Nevada through 2024. To check out wage data for Nevada by region and county, feel free to take a look at the table below that has the latest bls.gov statistics.
| Location | Pay Type | Low | Median | High |
|---|---|---|---|---|
| United States | Hourly | $12.05 | $18.29 | $30.21 |
| Yearly | $25,070 | $38,040 | $62,840 | |
| Nevada | Hourly | $12.80 | $20.31 | $30.94 |
| Yearly | $26,630 | $42,240 | $64,360 | |
| Las Vegas-Paradise, NV MSA | Hourly | $12.58 | $20.82 | $30.93 |
| Yearly | $26,180 | $43,300 | $64,340 | |
| Reno-Sparks, NV MSA | Hourly | $13.50 | $19.97 | $31.85 |
| Yearly | $28,080 | $41,540 | $66,250 | |
| Carson City, NV MSA | Hourly | $13.29 | $19.73 | $33.74 |
| Yearly | $27,640 | $41,030 | $70,190 | |
| Western Central Nevada BOS | Hourly | $12.80 | $18.81 | $25.62 |
| Yearly | $26,620 | $39,130 | $53,290 | |
| Other Nevada BOS | Hourly | $14.05 | $17.41 | $27.65 |
| Yearly | $29,210 | $36,210 | $57,510 |

