If you decide to become a medical biller and coder in one of the accredited medical coding and billing programs in Maryland, you can start a career in a medical field that is one of the quickest-growing in the entire country. Not only medical coding is growing in Maryland, but almost all healthcare careers in Maryland are too! It could not be a more exciting time to enter the allied health fields in Maryland! See all the details below with our latest guide to training.
Becoming a medical biller or coder in Maryland
All medical billers and coders in Maryland do not have to become certified to be employed but employers may demand it. That being said it is a good idea to be certified as soon as you can. The field itself is regulated at a national level and the certifying bodies are broken down in more detail here for you. We are not going to leave any detail out and only ant you to have all the information you need to succeed.
Find Medical Billing and Coding Programs in Maryland
What is the process for becoming a certified coding and billing specialist in Maryland?
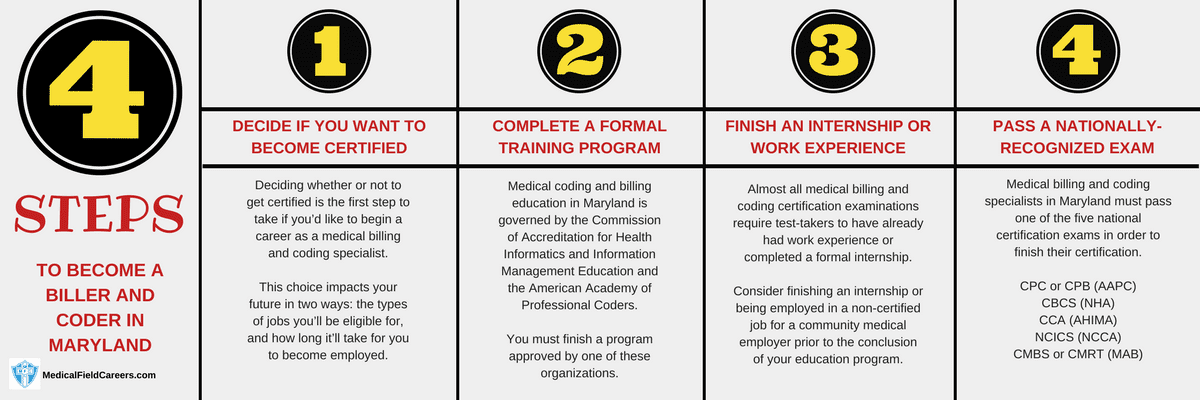
The exact process to become a medical biller or coder in Maryland is detailed below in the following four steps.
Step 1 – Determine if you are going to get certified in Maryland in Medical Coding and Billing
It is not mandated by the state of Maryland to be certified as a medical coder to get a job in the field of insurance reimbursement and billing. But, it will give you the best chance to get a job and make the best salary. Certification in medical insurance billing and coding in the state of Maryland cannot be undersold in anyway. It will only benefit your career for the positive and will help in the short term and long term for you too.
Step 2 – Complete a Maryland Medical Coding and Billing Specialist Training Program
Deciding on whether to get a bachelors degree, an associates degree or a certificate in medical coding in Maryland is the next choice that has to be made. Each has advantages and drawbacks to them.Mae sure you understand the timelines for your education levels. Certificates will take 6 months to a year to complete, associates degrees take 2 years in most cases and a bachelors degree usually takes a minimum of 4 years in the state of Maryland.
How to pick a Maryland billing and coding program
Picking a good medical insurance coding and billing program can be easy if you just follow this one rule. Sort schools in Maryland by the factor that matters the most to you and you will see the selection almost makes itself.
Approved Coding and Billing Schools in Maryland
All-State Career-Baltimore 2200 Broening Hwy Ste 160, Baltimore, Maryland 21224
Baltimore City Community College 2901 Liberty Heights Avenue, Baltimore, Maryland 21215
Fortis College-Landover 4351 Garden City Drive, Landover, Maryland 20785
Fortis Institute-Baltimore 6901 Security Blvd Ste 21, Baltimore, Maryland 21244
Hagerstown Community College 11400 Robinwood Dr, Hagerstown, Maryland 21742-6514
Purdue University Global-Hagerstown 18618 Crestwood Drive, Hagerstown, Maryland 21742
Step 3 – Make Sure to get an internship or work experience in Maryland for Coding and Billing
A requirement for many of the coding and billing certification exams offered in the state of Maryland is that the applicant needs to have already had job experience or finished a professional internship. Make sure to include this in your school selection process and bring it up at enrollment. It will really help you. The internship programs in Maryland are great ways to get access to career preparation that typical school programs in medical coding cannot give you.
Step 4 – Successfully pass the medical coding certification assessment for Maryland
Medical billing and coding specialists in Maryland are required to pass a national certification test to earn their certification in the state.
Click here for more details about the certification exams. At the link shown you will see what exam prep should be like, what the day of the exam will be like, what will actually be on the exam itself and more.
Medical biller and coder salary and jobs in Maryland
In Maryland the growing demand is extremely high for medical billing and coding specialists. Through the year 2024, the United States Bureau of Labor Statistics projects a 20% growth in new jobs for medical billing and coding specialists in the state of Maryland. The common Maryland workplaces are going to be at hospitals, physicians offices and general care facilities. Income data for Maryland coders and billers by region and county is on the table below that uses only the latest data from bls.gov.
| Location | Pay Type | Low | Median | High |
|---|---|---|---|---|
| United States | Hourly | $12.05 | $18.29 | $30.21 |
| Yearly | $25,070 | $38,040 | $62,840 | |
| Maryland | Hourly | $13.61 | $22.53 | $35.75 |
| Yearly | $28,320 | $46,850 | $74,360 | |
| Baltimore-Towson, MD MSA | Hourly | $13.58 | $22.75 | $36.09 |
| Yearly | $28,240 | $47,310 | $75,070 | |
| Washington-Arlington-Alexandria, DC-VA-MD-WV Metropolitan Division | Hourly | $12.74 | $20.32 | $34.86 |
| Yearly | $26,490 | $42,260 | $72,510 | |
| Hagerstown-Martinsburg, MD-WV MSA | Hourly | $13.82 | $19.78 | $29.11 |
| Yearly | $28,740 | $41,140 | $60,550 | |
| Wilmington, DE-MD-NJ Metropolitan Division | Hourly | $13.55 | $18.51 | $28.73 |
| Yearly | $28,170 | $38,510 | $59,750 | |
| Salisbury, MD MSA | Hourly | $12.20 | $17.33 | $27.39 |
| Yearly | $25,370 | $36,050 | $56,970 |

