The growth of allied health careers in tremendous and medical billing courses in Idaho are no different! See what the overall demand is and how the future is very bright for the coding and billing field with our latest article below. Healthcare careers across Idaho are seeing amazing growth and we love the fact that medical insurance coding and billing are seeing tremendous growth in Idaho too. We cover the details and steps to get certified in the state of Idaho as well as how to get started as soon as possible! Lets get started and not waste any time!
How to become a medical coder or biller in Idaho
Medical billers and coders are not required to hold a certification in order to work in the state of Idaho but it is highly recommended. The medical billing and coding profession in Idaho and across the nation is regulated on the national level. Here is a link to more details about the national regulating bodies. Do not miss any information that we make available to you. We want you fully informed when you make any school choice or decisions.
Find Medical Billing and Coding Courses in Idaho
What is the process for becoming a certified coding and billing specialist in Idaho?
Becoming a medical biller or coder in Idaho can be shown in the following four steps below.
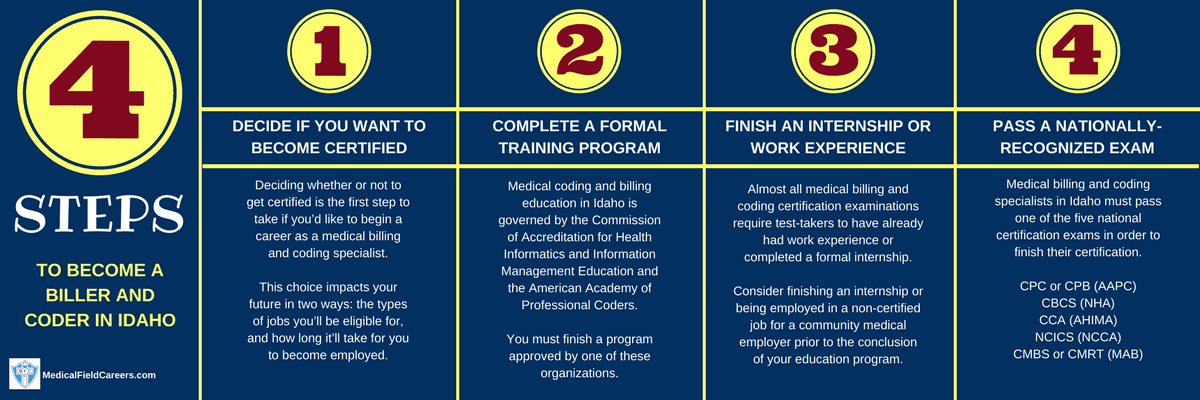
Step 1 – Decide if you are going to get certified in Idaho as a Medical Billing Specialist
In the state of Idaho it is not mandated that you be certified to work as a medical biller or coder. But remember, there are far more pros than cons to holding a certification. Also, most employers now demand that their staff get certified and even though there are some employers in Idaho that hire non-certified employees, it is not as many as that do hire certified workers. Do not let the process of certification or whether you should get certified be misunderstood in anyway shape or form. You only benefit from getting certified in Idaho as a medical coder. There really are no downsides beside the extra time studying and taking the examination.
Step 2 – Complete a Training Program in Medical Coding in the State of Idaho
Whether you get an associate degree, a bachelor’s degree, or a certificate, all three of them help you get your first medical coding and billing job in the state of Idaho, but you will need to be aware of the advantages and drawbacks of each before choosing one. For more details about the three levels of education, see our resource here. Each level has different time-frames from 6 months to 4 years depending on which level of education you go for.
How to pick a Idaho billing and coding program
Approved Idaho Medical Coding and Billing Schools
Lewis-Clark State College 500 8th Ave Lewiston ID 83501 208-792-5272
North Idaho College 1000 West Garden Avenue Coeur D’Alene ID 83814 208-769-3300
Carrington College-Boise 1122 N. Liberty St. Boise ID 83704 208-377-8080
Step 3 – Do an internship or get job experience in the state of Idaho
The state of Idaho has many employers that assist aspiring coders and billers with their training, make sure you check with your school if they offer any internship programs or work experience programs. Getting certified demands it in most situations. And it will also do wonders for your career growth. Internships are valuable ways to get access to the career early and will only help you get on the best career path possible. Do not underestimate the value of an internship in the state of Idaho!
Step 4 – Complete the official Coding and Billing Certification Path in Idaho
The official medical coding and billing certification tests used in Idaho are the five main national tests. These exams include segments on all important areas of knowledge you would have studied in your study course. The most-popular major national certification examinations recognized in Idaho are detailed here. From how to prepare for the exam, how to prep for the day of the exam, what to expect on the actual test and more!
Medical biller and coder salary and jobs in Idaho
The need for medical coding and billing specialists is at historic levels in Idaho. The Bureau of Labor Statistics in the United States expects a 15% increase in brand new positions nationally and a 17% increase in the State of Idaho through 2024. To review income statistics for Idaho by region and county, please check out the table below that only uses the latest bls.gov data.
| Location | Pay Type | Low | Median | High |
|---|---|---|---|---|
| United States | Hourly | $12.05 | $18.29 | $30.21 |
| Yearly | $25,070 | $38,040 | $62,840 | |
| Idaho | Hourly | $11.67 | $16.76 | $24.85 |
| Yearly | $24,270 | $34,870 | $51,680 | |
| Pocatello, ID MSA | Hourly | $14.94 | $20.43 | $27.83 |
| Yearly | $31,080 | $42,490 | $57,880 | |
| Boise City-Nampa, ID MSA | Hourly | $12.82 | $17.73 | $25.09 |
| Yearly | $26,660 | $36,880 | $52,200 | |
| Coeur d'Alene, ID MSA | Hourly | $11.90 | $17.59 | $27.86 |
| Yearly | $24,750 | $36,600 | $57,950 | |
| Southcentral Idaho BOS | Hourly | $12.55 | $16.89 | $23.99 |
| Yearly | $26,110 | $35,140 | $49,910 | |
| Lewiston, ID-WA MSA | Hourly | $11.98 | $16.62 | $27.56 |
| Yearly | $24,910 | $34,560 | $57,330 | |
| Logan, UT-ID MSA | Hourly | $12.08 | $15.83 | $28.91 |
| Yearly | $25,130 | $32,920 | $60,130 | |
| East Idaho BOS | Hourly | $10.63 | $15.26 | $23.91 |
| Yearly | $22,110 | $31,740 | $49,730 | |
| North Idaho BOS | Hourly | $10.76 | $14.41 | $24.34 |
| Yearly | $22,370 | $29,970 | $50,640 | |
| Idaho Falls, ID MSA | Hourly | $10.08 | $12.15 | $18.80 |
| Yearly | $20,960 | $25,260 | $39,110 |

