If medical billing and coding courses in Arkansas are something you are interested in, see our latest resource below. We walk you through the process to licensing in Arkansas and what to do get started below. Along with that, we have extensive data from bls.gov and we show the future growth of the allied health field as a whole. Most healthcare careers in Arkansas are seeing tremendous growth across the board and medical coding is among the best!
Becoming a medical biller or coder in Arkansas
It is not required by law to hold a certification in order to work in Arkansas but in most of the state, employers do prefer to hire certified individuals. The medical billing and coding profession in Arkansas is regulated on a national level. Certifications for billing and coding are recognized from several different national bodies Which we detail in a great resource here.
Find Medical Billing and Coding Classes in Arkansas
What is the process for becoming a certified coding and billing specialist in Arkansas?
The process for becoming a medical biller or coder in Arkansas is summarized in the four steps listed below.
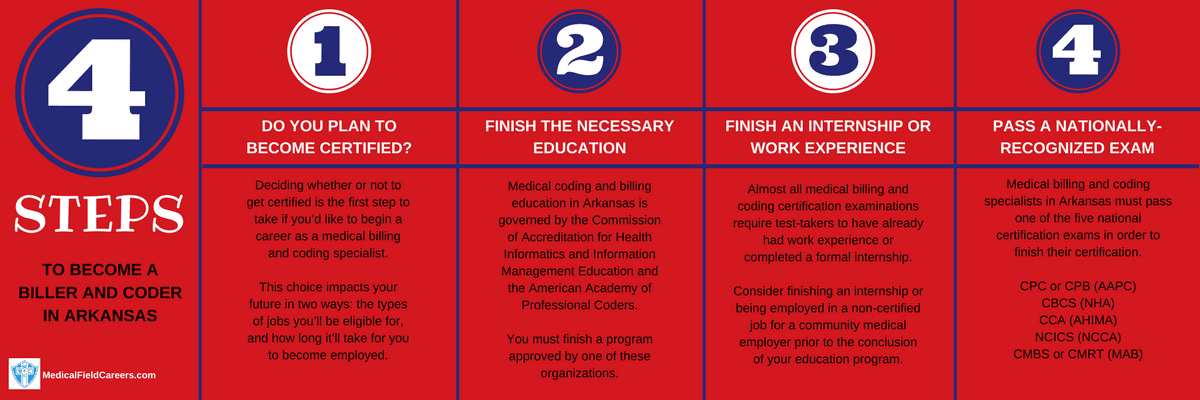
Step 1 – Determine if you plan to get certified in Arkansas as a Medical Coder
Although certification is not law in Arkansas it is highly recommended and should be considered strongly. The shift toward mandatory certification has additionally started to have an impact on non-certified personnel who have worked for many years. As a condition of continued employment, non-certified team members are often being ordered by employers to earn a certification. It is important to know that there are many benefits to getting certified and that they will get your career going in the right direction and have long term growth.
Step 2 – Finish an Accredited Arkansas Medical Billing Program
Whether it is a 4 year bachelors degree, a 2 year an associate degree, or a certificate that takes 6 months, all medical coders and billers in Arkansas must finish a formal education. For more details about the three options for education see our formal resource here. Most certificate diploma programs take a year at most to complete and it is most common for associate degree programs that are most often at community colleges to be two years in length.
What to search for in an Arkansas billing and coding program
To get good idea of the best options for medical coding training i the state of Arkansas you can do this one step we think is the best way. Sort all the schools by the most important factors to you and your education and after that the best schools will present themselves to you. It really does work that fast and easy!
Accredited Medical Billing and Coding Classes in Arkansas
Arkansas State University-Mountain Home 1600 South College Street Mountain Home AR 72653 870-508-6100
Arkansas Tech University Administration Bldg 200; 1509 N Boulder Ave Russellville AR 72801 479-968-0389
Blue Cliff College-Fayetteville 3448 N. College Fayetteville AR 72703 479-442-2914
Black River Technical College 1410 Hwy 304 East Pocahontas AR 72455 870-248-4000
South Arkansas Community College 300 S West Ave El Dorado AR 71731 870-862-8131
Arkansas Tech University Administration Bldg 200; 1509 N Boulder Ave Russellville AR 72801 479-968-0389
Step 3 – Complete an internship or acquire work experience in billing and coding
Since it is mandatory for students to get an internship or work experience for certification, coding and billing programs across Arkansas have partnered with local business employers oftentimes work together with accredited coding and billing programs to help arrange internships or work experience for students. Make sure you ask about these program opportunities when selecting your school of choice. Internships cannot be overlooked and should always be considered as a great opportunity.
Step 4 – Successfully pass a Medical Billing Specialist Certification Exam in Arkansas
In the State of Arkansas, you are required to pass one of the nationally-recognized examinations for medical coding and billing certification. For more information about what is in the national billing and coding exams see our resource here, it breaks it all down.
Medical billing and coding salary and jobs in Arkansas
The need for medical coding and billing specialists is at historic levels and the state of Arkansas is seeing growth like that as well. The Bureau of Labor Statistics expects a 15% growth in new jobs across the country and 17% incease in the State of Arkansas through 2024. To compare pay data for Arkansas by region and county, please take a look at the table below. All the data in the table below is from bls.gov.
| Location | Pay Type | Low | Median | High |
|---|---|---|---|---|
| United States | Hourly | $12.05 | $18.29 | $30.21 |
| Yearly | $25,070 | $38,040 | $62,840 | |
| Arkansas | Hourly | $9.97 | $14.85 | $24.00 |
| Yearly | $20,740 | $30,880 | $49,920 | |
| Memphis, TN-MS-AR MSA | Hourly | $11.34 | $19.00 | $33.96 |
| Yearly | $23,600 | $39,510 | $70,630 | |
| Little Rock-North Little Rock-Conway, AR MSA | Hourly | $11.46 | $18.00 | $26.35 |
| Yearly | $23,830 | $37,440 | $54,810 | |
| Texarkana, TX-Texarkana, AR MSA | Hourly | $10.65 | $16.79 | $34.67 |
| Yearly | $22,150 | $34,920 | $72,110 | |
| Hot Springs, AR MSA | Hourly | $10.33 | $15.76 | $19.03 |
| Yearly | $21,480 | $32,780 | $39,590 | |
| East Arkansas BOS | Hourly | $9.97 | $14.78 | $24.24 |
| Yearly | $20,750 | $30,750 | $50,430 | |
| Central Arkansas BOS | Hourly | $10.11 | $14.74 | $20.65 |
| Yearly | $21,020 | $30,670 | $42,950 | |
| Fayetteville-Springdale-Rogers, AR-MO MSA | Hourly | $10.14 | $13.65 | $23.55 |
| Yearly | $21,100 | $28,400 | $48,980 | |
| Pine Bluff, AR MSA | Hourly | $10.10 | $13.51 | $25.74 |
| Yearly | $21,010 | $28,100 | $53,540 | |
| Jonesboro, AR MSA | Hourly | $10.23 | $13.37 | $24.95 |
| Yearly | $21,280 | $27,800 | $51,900 | |
| South Arkansas BOS | Hourly | $9.33 | $13.16 | $18.77 |
| Yearly | $19,400 | $27,370 | $39,050 | |
| West Arkansas BOS | Hourly | $9.06 | $12.76 | $23.03 |
| Yearly | $18,840 | $26,550 | $47,900 | |
| Fort Smith, AR-OK MSA | Hourly | $8.87 | $11.87 | $18.24 |
| Yearly | $18,440 | $24,680 | $37,940 |

